November 6, 2025

Chronic insomnia affects millions of people, and it’s far more than just a frustrating night or two without sleep. For those who experience it, insomnia becomes a relentless cycle: the desperation to sleep intensifies anxiety, which makes sleep even harder to achieve. This is exactly what happened to my adult son during a particularly stressful period at work. After weeks of trying over-the-counter remedies, he asked his doctor for help and was prescribed a Z-drug and discovered that traditional medications come with their own troubling trade-offs. He took it for just one night and told me he had the most horrific nightmares he has ever experienced – nightmares that left him feeling shaken for days afterwards, they were so terrifying. On top of that, he felt completely drained the next day – unable to concentrate or function effectively.
You may be in the same boat: struggling with insomnia despite trying everything, including good sleep hygiene, cognitive behavioral therapy for insomnia (CBTi), and reducing screen time. You may have added magnesium and melatonin to no avail or tried over-the-counter sleep aids like Benadryl® or ZZZquil™ out of desperation, only to find they helped you fall asleep but not to stay asleep. Out of options, you are considering talking to your doctor about prescription medications but are afraid of potential side effects. Here’s what you should know: the risks go beyond what you feel tomorrow morning, long-term use of some pharmacological sleep aids carries significant hidden consequences.

Over-the-counter medications that contain diphenhydramine (Benadryl®, ZZZQuil™), or dimenhydrinate (Gravol™) inhibit the function of acetylcholine, a critical neurotransmitter involved in memory and cognition. While these medications have not been specifically studied in the context of dementia, research shows that regular use of “anticholinergics” for three years or more in those 65 and older is associated with a 54% increased dementia risk, and decreases in physical performance measures associated with frailty in seniors [1,2]. Dementia risk doubled in seniors 75 and older who had been using anticholinergics for 4.5 years [3].
Traditional prescription sedatives like Ambien® (zolpidem), benzodiazepines, and off-label use of drowsiness-inducing antidepressants carry significant risks. Side effects often include parasomnias (nightmares, sleepwalking, sleep talking, sleep paralysis) and daytime drowsiness. Long-term benzodiazepine use risks developing dependency and has been associated with a 60% increased risk of all-cause mortality, and longer-term risks for falls and dementia, particularly in older adults [4,5]. Z-drugs like zolpidem, eszopiclone, and zaleplon have such a high risk of inducing parasomnias that they actually carry a warning about increased risk of injuries causing death [6]. Long-term off-label use of low-dose sedating antidepressants for insomnia (e.g. trazodone) carries risks including physical dependence with withdrawal symptoms upon discontinuation, cardiac arrhythmias, orthostatic hypotension (dizziness on standing up), increased bleeding risk, and rebound insomnia after stopping.
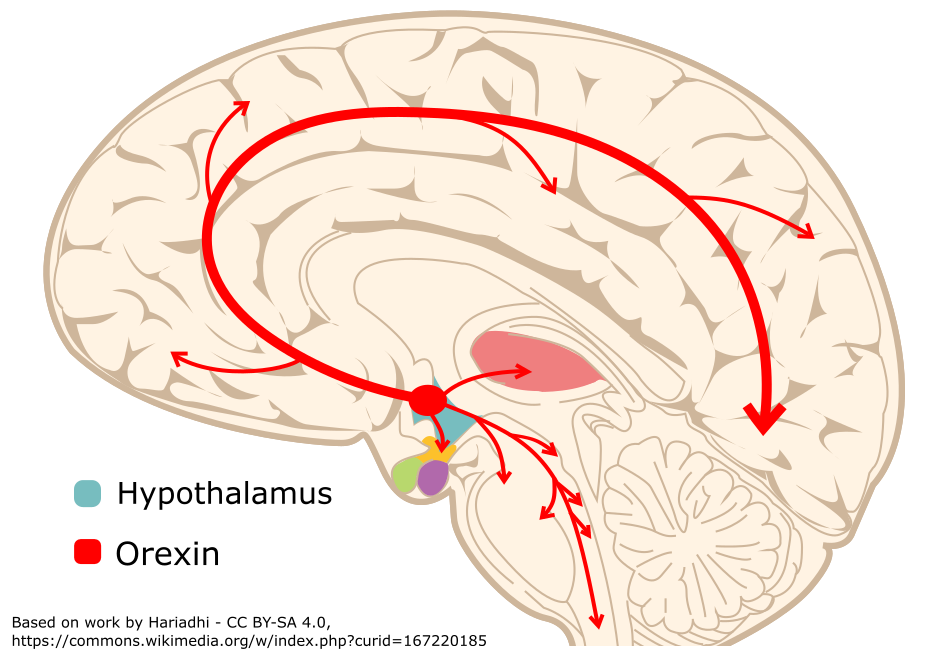
While Cognitive Behavioral Therapy for Insomnia (CBTi) is the best, most proven first-line treatment, it is often expensive and waitlists for therapists can be prohibitively long. Dual Orexin Receptor Antagonists (DORAs) are a new class of medications that represent a fundamentally new approach to pharmacological insomnia treatments by working with your body’s natural sleep-wake system.
Orexin is a neurotransmitter that actively promotes wakefulness. DORAs (including daridorexant (Quviviq®), lemborexant (Dayvigo®), and suvorexant (Belsomra®)), work by blocking orexin receptors, allowing sleep to occur naturally rather than forcing drowsiness. This is genuinely different from benzodiazepines or older medications that broadly suppress brain activity by enhancing GABA function.
The evidence is cautiously compelling. Clinical trials demonstrated that, compared to placebo, DORAs significantly increase total sleep time, reduce the time it takes to fall asleep, and reduce the number of times people wake up after sleep onset (and how much they are awake in the night) [7,8]. Critically, unlike traditional sedatives, DORAs preserve REM sleep duration which is essential for emotional regulation and memory consolidation [9]. A network meta-analysis comparing 7 different sleep medications found that in terms of risk/benefit, orexin antagonists were a recommended option for both short and long-term treatment of primary insomnia, and safe for elderly patients [10].
Common side effects are mild, such as headache, somnolence, vivid dreams, and nasopharyngitis [8]. The risk of daytime drowsiness varies by medication half-life: Daridorexant has an 8-hour half-life (lower daytime drowsiness risk), while lamboerxant has a 12–17-hour half life (better for sleep maintenance insomnia, but greater risk of daytime drowsiness).
DORAs aren’t without limitations. They’re newer medications (FDA and Health Canada-approved within the last decade), so long-term outcome data is still accumulating, and they can take up to 4 weeks to really kick in. They’re also more expensive than traditional options.
Cost is a significant barrier for many patients, including Canadians: Canada’s Drug Agency (CDA-AMC) recommended against reimbursement for daridorexant (Quviviq®) and Lemborexant (Dayvigo®) the only two currently Health Canada-approved DORAs.
These denials are deeply frustrating for Canadian patients desperately seeking better options. Without public funding, DORAs remain financially inaccessible for many.

If behavioral approaches haven’t solved your sleep problem, and you’re considering medication, DORAs represent a new option with potentially fewer risks and reduced side-effects: they avoid the dementia risks of anticholinergics, the dependency issues and fall risks of benzodiazepines, and the intense parasomnias of z-drugs.
Start by discussing with your healthcare provider whether a DORA is appropriate for your specific situation. If you’ve been taking other sleep medications, allow sufficient time between switching to a DORA to avoid rebound and interaction effects, including parasomnias like sleepwalking and nightmares. Be particularly cautious if you are taking other medications that affect the central nervous system, since there haven’t been sufficient studies on DORA drug-drug interactions.
Many patients and even some healthcare providers aren’t yet aware that this class of medications exists. Most of the conversations around insomnia still revolve around traditional treatments, leaving many to assume they’ve exhausted their options. As awareness of DORAs grows, patients and clinicians alike can make more informed decisions about when and how these therapies fit into the broader landscape of sleep health.
*Disclaimer: This article is for informational purposes only and does not constitute medical advice. The mention of specific companies, products, or organizations in this article is for informational purposes only and does not imply endorsement. The companies whose products were referenced were not consulted, involved in the preparation of this content, nor did they provide any funding or compensation.
[2] S. L. Gray, Y.-R. Su, T. C. Eshetie, A. Z. LaCroix, Z. A. Marcum, and O. Yu, “Cumulative Anticholinergic Exposure and Change in Gait Speed and Grip Strength in Older Adults,” JAMA Netw. Open, vol. 8, no. 7, pp. e2519819–e2519819, Jul. 2025, doi: 10.1001/jamanetworkopen.2025.19819.
[3] F. Jessen et al., “Anticholinergic drug use and risk for dementia: target for dementia prevention.,” Eur. Arch. Psychiatry Clin. Neurosci., vol. 260 Suppl 2, pp. S111-5, Nov. 2010, doi: 10.1007/s00406-010-0156-4.
[4] K. Y. Xu, S. M. Hartz, J. T. Borodovsky, L. J. Bierut, and R. A. Grucza, “Association Between Benzodiazepine Use With or Without Opioid Use and All-Cause Mortality in the United States, 1999-2015,” JAMA Netw. Open, vol. 3, no. 12, pp. e2028557–e2028557, Dec. 2020, doi: 10.1001/jamanetworkopen.2020.28557.
[5] K. L. Stone, K. E. Ensrud, and S. Ancoli-Israel, “Sleep, insomnia and falls in elderly patients,” Sleep Med., vol. 9, pp. S18–S22, 2008, doi: https://doi.org/10.1016/S1389-9457(08)70012-1.
[6] K. Harbourt, O. N. Nevo, R. Zhang, V. Chan, and D. Croteau, “Association of eszopiclone, zaleplon, or zolpidem with complex sleep behaviors resulting in serious injuries, including death.,” Pharmacoepidemiol. Drug Saf., vol. 29, no. 6, pp. 684–691, Jun. 2020, doi: 10.1002/pds.5004.
[7] T. Kishi et al., “Comparative efficacy and safety of daridorexant, lemborexant, and suvorexant for insomnia: a systematic review and network meta-analysis.,” Transl. Psychiatry, vol. 15, no. 1, p. 211, Jun. 2025, doi: 10.1038/s41398-025-03439-8.
[8] H. Liu et al., “Efficacy and safety of insomnia pharmacotherapies: Convergent evidence from Bayesian network meta-regression and FAERS-based disproportionality analysis.,” Sleep Med., vol. 136, p. 106848, Oct. 2025, doi: 10.1016/j.sleep.2025.106848.
[9] D. Sarathi Chakraborty, S. Choudhury, and S. Lahiry, “Daridorexant, a Recently Approved Dual Orexin Receptor Antagonists (DORA) in Treatment of Insomnia.,” Sleep Sci. (Sao Paulo, Brazil), vol. 16, no. 2, pp. 256–264, Jun. 2023, doi: 10.1055/s-0043-1770805.
[10] L. Wang et al., “A network meta-analysis of the long- and short-term efficacy of sleep medicines in adults and older adults,” Neurosci. Biobehav. Rev., vol. 131, pp. 489–496, 2021, doi: https://doi.org/10.1016/j.neubiorev.2021.09.035.